On an October evening in 2014, Ilana Massi and her husband Bob were planning to watch a baseball game when Ilana felt ill. She felt weak and her fever was spiking, so they drove to the hospital near their suburban Los Angeles home. When her blood work came back, Massi, a trained nurse, didn’t need a doctor to tell her what was wrong. She looked at her husband and said, “Those are leukemia numbers.”
A diagnosis of acute myeloid leukemia (AML)
At that point, Massi says, she had one single wish: Please don’t let it be AML. As a nurse, she knew all about AML, the most deadly form of blood cancer.1 Coincidentally, the youngest of her five sons, Evan, was a research associate at the University of California, San Francisco who happened to be researching the genetic roots of the disease. In patients with AML, the blood factories in the bone marrow produce blasts of large, malignant white blood cells, which crowd out healthy blood cells.2 Occurring with terrifying speed, the disease can progress very quickly.2 While there have been recent developments in AML research and understanding, the current five-year survival rate remains just 27% in the US.3
Massi’s worst fear came true. As soon as they diagnosed her with AML, doctors rushed her into an intense round of chemotherapy, hoping to stem the rising tide of mutated, harmful white cells in her body and save her life. “They didn’t think I’d survive the first week,” she says.
The long road to recovery
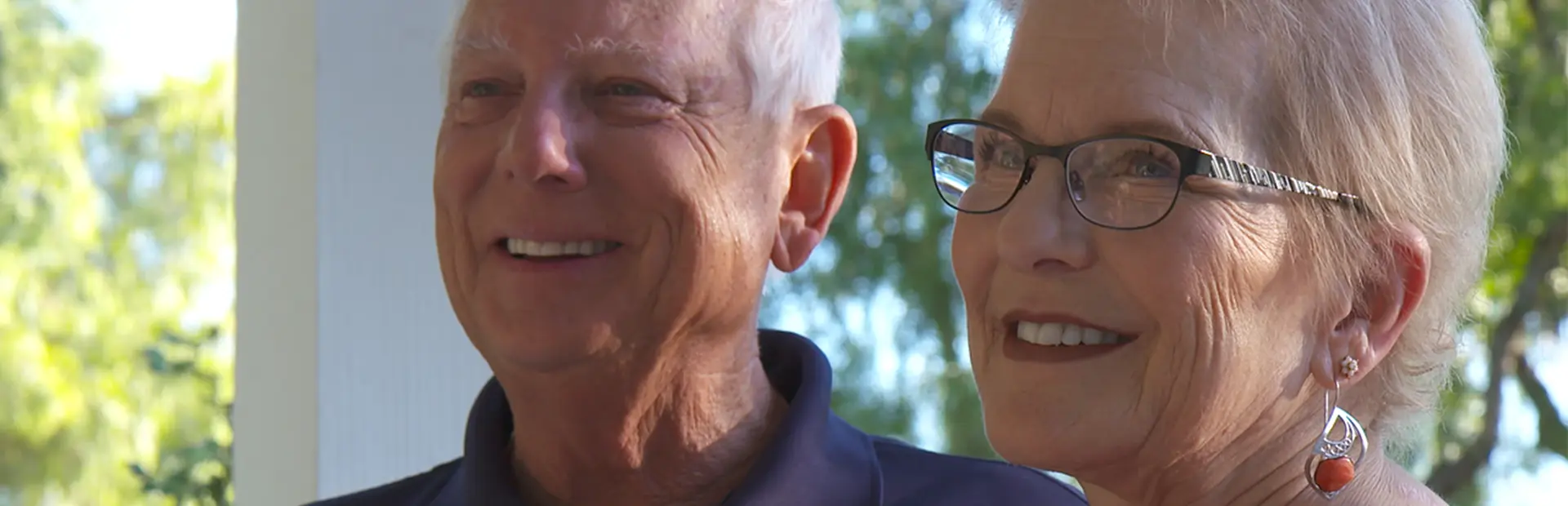
Massi made it. However, her trip to the emergency room began a long and harrowing voyage that continues to this day. Recounting her journey from her home in Thousand Oaks, California, her voice catches with emotion as she recalls not only the fear and pain she experienced, but also the support she received from her family, friends, doctor and nurses – and especially from the stem cell donor whose blood-forming stem cells saved her life. “He's like another son to me,” she says.
As soon as they diagnosed the AML, doctors rushed her into an intense round of treatment, hoping to stem the rising tide of mutated, harmful white cells in her body, and save her life.
Massi’s ordeal began with five full months in the hospital. There she received a crucial stem cell transplant and then began an exhausting new battle to keep the donor stem cells that circulate in her body from launching an attack on her organs (a phenomenon called graft-versus-host disease). New problems crop up with frightening regularity. “It's like whack-a-mole,” she says.
When she fell ill, Massi was an 18-year veteran of the pharmaceutical industry, where she worked in medical affairs. She understood what was happening to her with both the disease and the punishing treatments. Massi was also well versed in common patient reactions: feelings of grief, powerlessness, anger and despair. But this knowledge didn’t prevent those feelings from bubbling up. “I was so mad,” she recalls. “I thought I wasn’t going to see my grandson.”
A lifeline of support
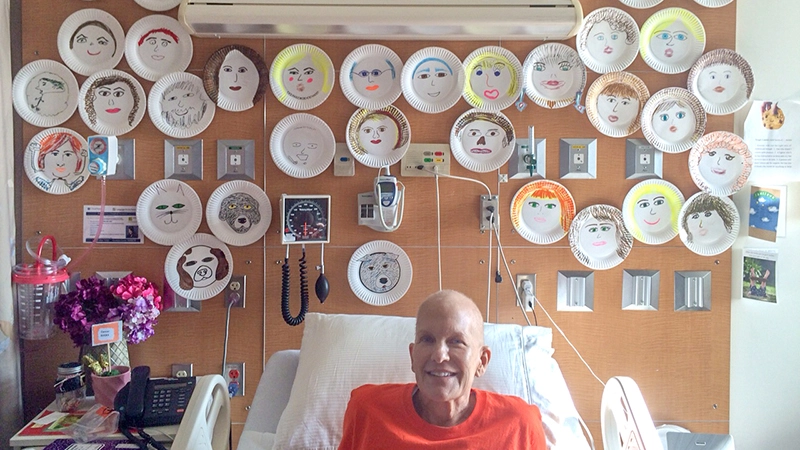
What carried her through her darkest days was a steady stream of support from neighbors, colleagues, friends and family. It extended far beyond texts and emails. They donated blood and she tracked their donation numbers so she was aware if she had received a transfusion from someone she knew. Knowing that she was feeling lonely, scared and depleted, more than 200 of her friends – including her colleagues at Novartis – painted their faces on paper plates and shipped them to her in the hospital. Massi had them taped to her hospital wall. The constellation of friendly faces smiled down at her, reminding her that she was not alone. “I can’t tell you how good it made me feel to see all those faces,” she says.
Her battle with AML has changed her. She has less energy and has to prioritize where she spends it. “She was always a type A,” says her husband. As a mother, a wife and a professional, she was always in control and determined to be the best. Now she cedes more to others. “She’s probably a type B now, or C.”
Their son Evan notices his mother’s fondness for the small details in life, such as special moments and human connections. He recalls one of their first family dinners after her transplant. “She looked around the room a lot, taking it in,” he says. “I think she just appreciated being in the world.”
The constellation of friendly faces smiled down at her, reminding her that she was not alone.
Helping the AML community
These days, Massi works to provide support for the more than 20,000 people diagnosed with AML every year in the US.4 The disease strikes a similar number in Europe5 and accounts for about one-quarter of adult leukemia cases worldwide.1 She now works with a health organization as a patient-family outreach coordinator, welcoming the newly diagnosed and their families, and helping them with services and information.
Her other objective as an advocate is to be part of the “loud patient lobby” for the disease. When patients and their supporters make noise, she says, regulators and pharmaceutical companies hear them and are more likely to push research and move medications through the pipeline. What’s more, a loud lobby raises awareness about AML, which can lead more people to join bone marrow donor registries.
For AML patients, finding a closely matched donor is often a matter of life or death. For Massi, it was a dangerously close call. Her cancer stubbornly resisted repeated batteries of chemotherapy and radiation for two months. She needed the AML to go into remission for a transplant to take hold and save her life.
Continued treatment
In January 2015, three months after her diagnosis, Massi’s leukemia finally went into remission. But she had trouble finding a donor. None of her three sisters matched her relatively rare blood type. In the entire donor registry, only seven people were matches for Massi, and most of them were outside the US.
Her most promising stem cell donor, an anesthesiologist based in New York, wasn’t a perfect fit. Of the 10 genes doctors analyzed, nine of his matched Massi’s. If doctors had the luxury of time, they might have waited for a perfect 10, which would lessen the risk of donated cells attacking the body.
Massi’s oncologist, Dr. Pablo Parker, worried that her leukemia would return any day. “Sometimes you lose the window,” he says. He knew that Massi, like many AML patients, had a genetic mutation that spurred on the disease. In recent years, researchers have identified a handful of such mutations. Some of them turn off the genes that suppress tumors and help the body fight cancer. Others, like Massi’s, become so-called oncogenes, which drive the growth of cancer. Much of the research into AML and other cancers is focused on targeting these cancer-driving mutations and changing their behavior.
Massi’s genetics made it much more likely that her remission would be short-lived. If the cancer returned, her hopes for a transplant would fade – and that was her only shot. So her medical team prepared her for a transplant and then infused the donor’s stem cells into her bloodstream. Those cells quickly made their way into the bone marrow, and within several days they were producing healthy blood cells and platelets.
A few months later, Massi was able to meet her grandson, Jameson, whom she feared she’d never see. According to her husband, “That made an incredible difference for her. You love your own children, but for some reason a grandchild is a whole different kind of love.”
A new normal
Life now is very different for Massi. She takes 20 medications a day, most of them to battle graft-versus-host disease, which she developed following her transplant. She’s easily fatigued and suffers from skin and stomach trouble. Her hair had started to grow back, but then stopped.
In the future, she hopes AML patients will have medications that target the genetic mutations that cause AML to develop. Perhaps they’ll be spared the ordeal of chemotherapy, radiation and bone marrow transplants. Massi wouldn’t wish her situation on anyone. But she’s happy that she’s still alive today and closer to friends and family than ever.
Additional Resources
Inside one woman's fight against #AML.