The kidneys play a vital role in keeping us healthy, and it is often only when something goes wrong that we realize just how important they are.1 Unfortunately, as many as 1 in 10 people are affected by chronic kidney disease (CKD) worldwide, which occurs when the kidneys have been damaged over time and can no longer function the way they should.2
There are many different causes of CKD.2 In some rare kidney diseases, called complement-mediated kidney diseases, damage to the kidneys is caused when a part of the immune system becomes overly active.3-5 This generates an inflammatory response that leads to kidney damage, resulting in protein in the urine (proteinuria) and lower kidney function.3,5

Types of complement-mediated kidney diseases
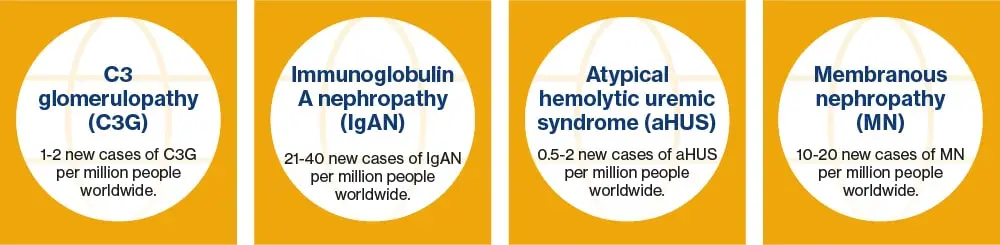
Complement-mediated kidney diseases are chronic, rare, complex and progressive and occur when the immune system becomes overly active.3-9 They include diseases such as C3 glomerulopathy (C3G), IgA nephropathy (IgAN), atypical hemolytic uremic syndrome (aHUS) and membranous nephropathy (MN).7-10
These rare kidney diseases, with the exception of MN, can start early in life, mainly affecting teens and young adults, though symptoms may not be noticed until later in life.11-14 Unfortunately, some patients will progress to kidney failure within only 10 years of being diagnosed.7,15-21
Living with complement-mediated kidney diseases
People living with complement-mediated kidney diseases can experience a variety of symptoms, including debilitating fatigue, that have a significant impact on their quality of life.22-25 This can limit physical activities and abilities to socialize, resulting in severe psychosocial consequences, including reduced motivation, depression and anxiety.23-25
Unfortunately, there are limited treatment options specifically approved for these rare kidney diseases.7,10,15,25-27 Oral corticosteroids and immunosuppressants can be used in patients at high risk of disease progression, but these often come with significant side effects, including hypertension, diabetes, obesity and a heightened risk of infections.25-28
