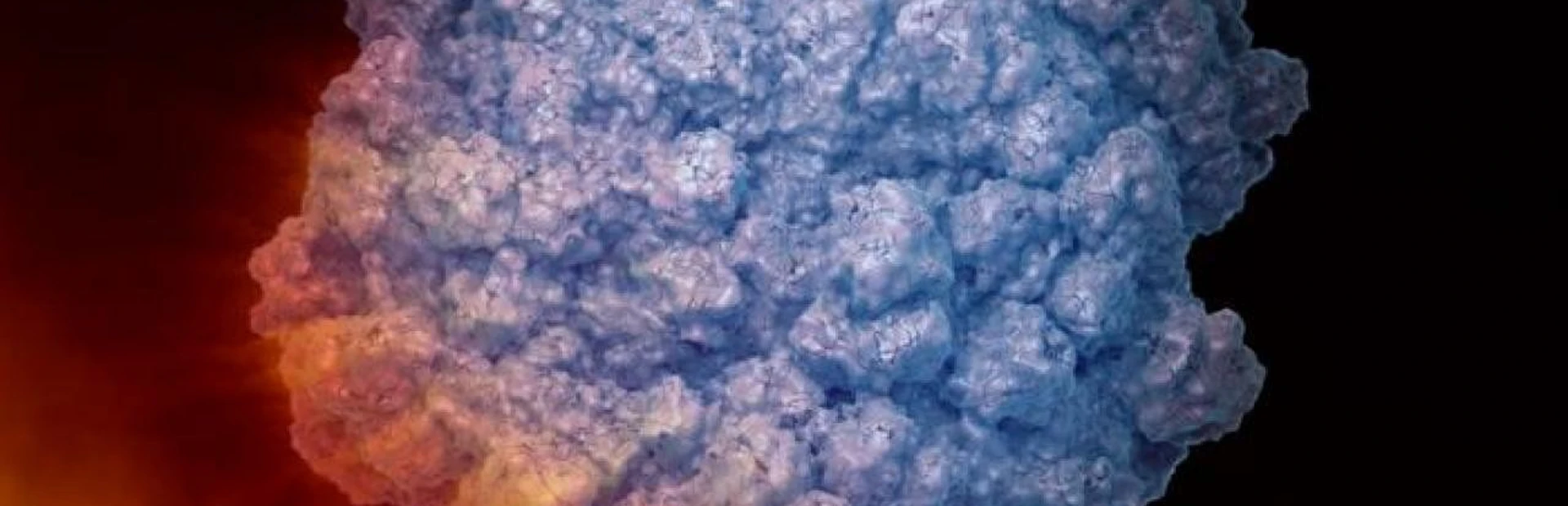
Cancer cells loaded with mutations are prime targets for your immune system, which right now is probably knocking off quite a few of your cells that are breaking bad.
Unfortunately, cancer also puts up many defenses, and by the time a tumor is big enough to be detected and treated, the immune system has lost the battle.
But maybe not the war.
One of the most promising concepts in cancer immunotherapy looks at tumors as “hot” or “cold” or somewhere in between, depending on how densely they are infiltrated by the immune system’s army of cells, says Steven Bender, Director of Oncology at the Genomics Institute of the Novartis Research Foundation in San Diego, California.
“The level of immune infiltration reflects whether the immune system is recognizing and engaging the tumor,” Bender says. And at least in some cancers, he adds, the hotter the tumor, the better the patient’s chances.
He points to a measure called the Immunoscore, based on the density of two types of T cells in a sample of the tumor. T cells are the main driver of the adaptive immune response. Some T cells retain a memory of their exact designated victims for years, and unleashing them is the main goal of most cancer immunotherapy.
Heat in the Immunoscore is a good predictor of outcomes for patients with colorectal cancer, as a recent review notes. “What that means is, if you are diagnosed with early stage colon cancer that is “hot” and have surgery to remove the primary tumor, your prognosis is good and your cancer will be unlikely to return,” Bender explains. “If it’s cold, your probability of relapsing is much higher.”
While the mechanisms underlying these results aren’t fully understood, scientists believe that in a hot tumor, the immune system stays engaged after the tumor is removed. It may have suppressed any metastases up to that point, or it may take care of business once the main tumor is removed, Bender says. But in a cold tumor, any metastases eventually will grow out because the immune system can’t see them.
The Immunoscore is a better predictor of cancer progression than other markers such as tumor stage or pathological grade, he adds. The study looked at colorectal cancer, but many researchers expect that this concept can be extended to other types of solid tumors.
Many scientists also hope that the concept of hot and cold tumors can be extended to a hot new class of immunotherapy drugs—“checkpoint inhibitors” designed to remove some of the immune system’s own self-control mechanisms that solid tumors put to grim use. So far, the new drugs tend to work best on cancers that tend to run hot on the immune scale, such as melanoma.
“Cold tumors are not very responsive to checkpoint inhibitors alone,” says Bender. “There’s just no immune engagement, so the inhibitor doesn’t take off the brakes.”
That recognition is leading many labs—including labs at Novartis—to look at ways to activate the immune system in patients with cold tumors, by generating what is called a type 1 interferon response, before giving the patients a checkpoint inhibitor. Learn about a collaboration that is advancing this research.
To fully exploit this approach, Bender emphasizes, we need a deeper understanding of what makes a cold tumor cold—what combinations of mutations in the tumor, mutations in the patient’s immune system genes, or perhaps other factors like environmental exposures might turn up or turn down the heat.