A new wave of therapies is unleashing the body’s immune system on cancer, significantly extending lives. These agents, however, don’t work for everyone, so scientists are exploring new approaches that might enable immunotherapies to more effectively combat tumors.
One idea, born of a team of bioengineers, involves loading baby-aspirin-sized scaffolds with immunotherapy agents and inserting them near tumors. These biodegradable scaffolds can potentially serve as “boot camps” for immune cells, recruiting and training them to recognize tumors and launch an attack. Novartis recently entered a licensing agreement with Harvard University and initiated a collaboration with the Wyss Institute at Harvard University and the Dana-Farber Cancer Institute in the US to explore the potential applications of this technology.
“The goal is to reprogram the immune landscape of tumors,” says Glenn Dranoff, Head of Immuno-oncology at the Novartis Institutes for BioMedical Research. “The scaffolds provide a site where key immune cells can mingle with compounds that we’ve selected to educate them.”
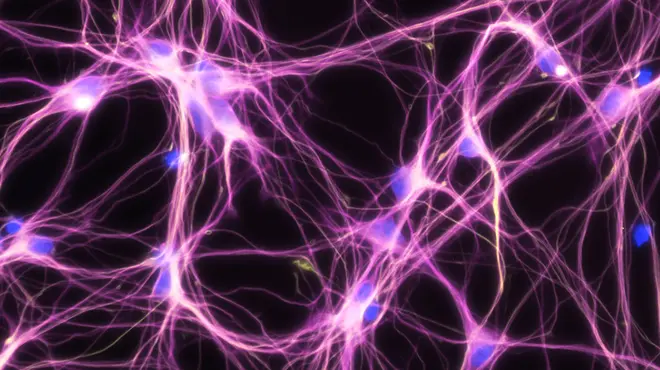
Like newly enlisted members of the military, immune cells have the potential to fight the enemy, but they often lack the training. These cells could benefit from being temporarily sequestered in a site devoted to their education. Prolonged exposure to multiple immunotherapy agents might give them an advantage in battle, enabling them to fight harder than cells that encounter such agents in a haphazard fashion.
In addition, the immune cells might ultimately perform better if they’re shielded from conflicting cues while being trained. Tumors often release signals that trick the immune system into thinking that everything is OK. By keeping such signals at bay, the scaffolds might enable immune cells to devote their full attention to the compounds in their immediate vicinity. Hopefully, they’ll have a better chance of realizing that the patient is in danger and of responding to the threat.
“The biodegradable scaffolds are porous,” explains David Mooney, who conceived of the technology. Mooney is the Robert P. Pinkas Family Professor of Bioengineering at Harvard John A. Paulson School of Engineering and Applied Sciences and a founding member of the Wyss Institute who conceived of the technology. “Once immune cells enter, we have control over the microenvironment, so we can provide them with the right cues while shielding them from systemic signaling.”
First-generation device
Mooney began developing the first scaffold 10 years ago, inspired by the body’s initial response to a local infection. Seeing that immune cells quickly flood to the site, Mooney wondered if he could build a device to mimic an infection near a tumor.
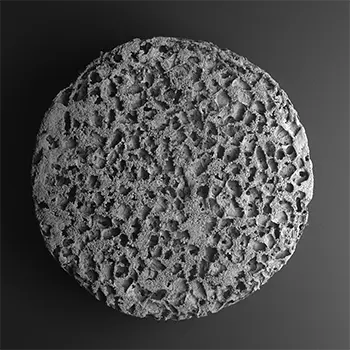
The first challenge was to find a safe material with the right properties for the device. Mooney settled on the porous polymer that’s used in biodegradable sutures, a tried-and-tested product.
Next, he collaborated with researchers at Dana-Farber to select a compound that would attract dendritic cells of the immune system. These “sentinels” monitor the body for threats and activate T- and B-cells – which can neutralize the enemy – when they encounter an invader. But dendritic cells must recognize the invader to do their job.
Once dendritic cells enter Mooney’s device, they are exposed to an antigen, a molecule that enables them to recognize the invader – tumor cells, in this case. The antigen can vary, depending on the type of tumor that’s being targeted. The device is also loaded with an adjuvant, a compound that enhances the reaction to the antigen.
The first-generation device is being tested in an early-phase clinical trial at Dana-Farber. It’s inserted surgically, requiring a small incision.
“We wanted to make it even easier to administer the device to patients, so we began working on injectable versions,” says Mooney.
Evolving technology
His group is pursuing two new strategies for the device. One involves using a cryogel, a highly elastic material with shape memory. The cryogel can be loaded with compounds, compressed and delivered via needle into the body, where it springs back to its original size. The other strategy involves microparticles that self-assemble after being injected into tissue.
Novartis will collaborate with Mooney and researchers at the Wyss Institute and Dana-Farber on further development of the technology. As part of this effort, the team will load the core scaffolds with different combinations of immunotherapy agents, including proprietary Novartis compounds. The researchers aim to test some of the combinations with the devices in clinical trials to determine if they can help cancer patients with intractable tumors.
“The intersection of materials science and immunology is a very exciting place for us to be,” says Dranoff. “It provides opportunities that were previously unimaginable. The use of biodegradable materials allows for improved spatial and temporal control over the release of our immunotherapy agents.”
Main image: A scientist at Harvard’s Wyss Institute holding a device that can be loaded with immunotherapy agents designed to fight tumors. Image courtesy of the Wyss Institute.
Novartis is collaborating with @wyssinstitute and @DanaFarber to develop devices with #cancer-fighting potential.